What is Immune-Mediated Thrombocytopenia?
The immune system is an extremely complex network of cells and tissues that protect animals from infection. When foreign invaders, such as a virus or bacteria, infect the host animal, that animal’s immune system recognizes potential danger. Many signaling processes occur that cause the cells of the immune system to target the foreign invader and eliminate it.
Immunity is typically a very efficient and effective process, but it is not perfect. During the early development of an animal before it is even born, the immune system learns which cells belong to the host animal’s body and should therefore never be attacked by the immune response. During an animal’s lifetime, the immune system may go awry for various reasons and erroneously misrecognize “self” cells as foreign. If this happens, the immune response will subsequently try to eliminate the misrecognized cells and thereby cause disease. This process is often described as an auto-immune disease.
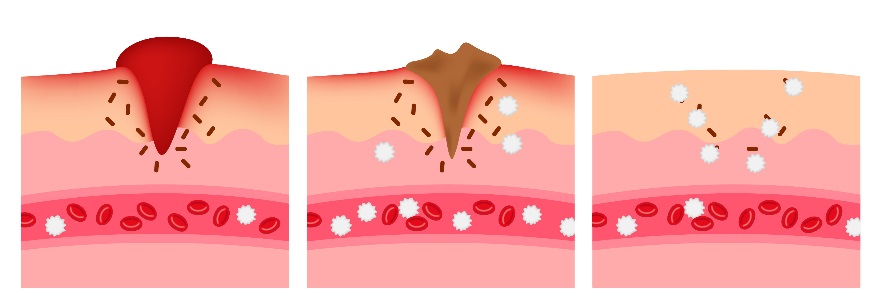
Immune-mediated thrombocytopenia (ITP) is an example of an auto-immune disease where the immune system destroys platelets within the body when they are misrecognized. Thrombocyte is another term for platelets. The term “-penia” indicates there is a deficiency in the number of cells.
Why Are Platelets So Important?
Platelets are a type of blood cell produced in the bone marrow and then released into the bloodstream. Their purpose is to assist with coagulation (the arrest of bleeding due to clot formation). When a blood vessel wall becomes damaged, platelets become activated and bind to each other to create a “platelet plug” to stop bleeding. Therefore, when platelet numbers are severely decreased, or the platelets are unable to function properly, the patient is at risk for uncontrolled bleeding.
When thrombocytopenia becomes severe, several clinical signs may become apparent. The patient may appear lethargic. Examination of the skin or gums may reveal small, pinpoint sites of bleeding called petechiation. Larger areas of bleeding called ecchymoses (essentially, bruises) may also appear. Nose bleeds, blood in the urine, or blood in the stool (often noted as black, tarry stool) are sometimes seen. Prolonged bleeding after a traumatic incident is also indicative of an issue with coagulation. Bleeding in other places might lead to other clinical signs; for example, bleeding into the eyes can cause blindness or bleeding into the brain can cause seizures.
These images illustrate petechiation on the gums and abdomen.
(Photos courtesy of Leah Cohn, DVM, PhD, DACVIM)
What Causes ITP?
- Primary ITP: Occurs without an identifiable underlying cause, and is likely due to a defect in the immune system.
- Common in dogs, rare in cats.
- Predisposing factors: age (young adults to middle aged dogs), breed (smaller dogs often affected but can be seen in any dog)
- Secondary ITP: The immune system destroys platelets because of underlying disease.
- Predisposing factors: drug administration, infection (especially tick-borne diseases), cancer, or other disorders.
It is important to remember that immune-mediated disease is not the only potential cause of thrombocytopenia. Below is a table summarizing several additional causes that must be considered:
| Infectious | Examples: canine distemper virus, parvovirus, feline leukemia virus, tick transmitted infections such as ehrlichiosis or Rocky Mountain Spotted fever, fungal infections, or bacterial infections |
| Neoplasia | Examples: multiple myeloma, lymphoma, leukemia, hemangiosarcoma |
| Drugs | Examples: antibiotics, chemotherapeutic drugs, estrogen |
| Hereditary | Examples: macrothrombocytopenia, seen in Cavalier King Charles spaniels and other breeds, greyhounds |
| Miscellaneous | Examples: splenic enlargement, disseminated intravascular coagulation, bone marrow disorders |
How is ITP Diagnosed?
Diagnosing an animal with platelet disease begins with a thorough history and physical examination.
A blood sample will be obtained to perform a platelet count. A count from a machine is not enough to confirm a low count because platelets may clump together in a blood sample causing it to seem low artificially. Therefore, a blood smear should be prepared and examined under a microscope by a trained expert. Microscopic analysis of a blood sample may reveal several characteristics of the platelets:
- The presence of platelet fragments is indicative of the immune system attacking the platelets
- Some heritable breed specific diseases that cause low platelet counts are recognizable on a blood smear
- Some infectious causes of a low platelet count are recognizable on a blood smear
Additional diagnostic tests can help rule in or rule out diseases that affect platelets. Because platelets come from the bone marrow, examining a bone marrow sample under the microscope may help determine if the cause of thrombocytopenia is due to an issue with platelet production. Additionally, there are several diseases that are contracted from ticks that may cause thrombocytopenia, so tests that rule out diseases from ticks are important to perform. Lastly, other components of coagulation unrelated to platelets may malfunction for various reasons. There are specific tests available to examine the status of these coagulation components. A diagnosis of ITP is typically made after excluding other causes for a low platelet count.
What Treatment Options are Available
- Immunosuppressive drugs: Steroids such as prednisone will help block the cell mediated destruction of platelets. If prednisone does not work or if the side effects are not tolerable, additional immunosuppressive drugs are available (eg. azathioprine, cyclosporine).
- Vincristine: This is a chemotherapy medication that can cause a temporary increase the number of platelets.
- Intravenous immunoglobulin: A blood product containing antibodies can cause a short-lived reprieve from rapid platelet destruction in some animals.
- Supportive care: This includes cage rest, exercise restriction, and eliminating any activities that would cause bleeding. Patients should be monitored closely for signs of spontaneous bleeding. In many cases, a blood transfusion may be required to replenish lost red blood cells. Very rarely, a special transfusion of platelets is also necessary.
What is the Expected Outcome for My Pet?
The prognosis for ITP ranges from good to guarded. Although almost 80 percent of dogs with this disorder will recover, that means that another 20 percent are either euthanized or die because of the disease. Several factors have been shown to effect prognosis. Patients with melena (blood in their stool), elevated kidney values on blood tests, or those who require a blood transfusion may have a harder time overcoming the disease.
Even for dogs that respond well, relapse may occur in the future. Research studies have demonstrated varying relapse rates ranging from 9 to 31 percent. Unfortunately, if a dog relapses once, there is about a 50 percent chance that it will occur again. Typically, the first relapse will occur within a year of the initial diagnosis.
Steroids are the mainstay of treatment for managing ITP, however these drugs are associated with several side effects. Much like people, animals receiving steroid treatment will have an increased appetite which may lead to weight gain. They will often exhibit increased thirst and urination. Administration of an excessive dose of steroids can lead to other disorders, too, therefore requiring careful monitoring. Additionally, although suppressing the immune system will help manage the ITP, it will also make the animal more susceptible to infections.
Fortunately, patients do not typically require immunosuppressive medication for life. Steroids are typically prescribed in a “tapering” dose, meaning that they are slowly decreased over several months. Repeat platelet counts should be performed whenever the dose of immunosuppressive medications is altered. Pet owners should be well informed of the clinical signs associated with thrombocytopenia, and cognizant of the importance of monitoring for those signs in the future.
Written by Eileen Donoghue, MU College of Veterinary Medicine Class of 2019